Narcolepsy is a chronic neurological disorder that affects the brain's ability to regulate sleep-wake cycles. People with narcolepsy often experience sudden and overwhelming episodes of drowsiness, known as "sleep attacks," which can occur during activities such as working, driving, or even while talking to someone. These sleep attacks can be disruptive and potentially dangerous. These episodes are called "narcoleptic sleep attacks."
Types of narcolepsy
There are two primary types of narcolepsy: narcolepsy type 1 (previously known as narcolepsy with cataplexy) and narcolepsy type 2 (previously known as narcolepsy without cataplexy). In addition to these two types, there is also a condition known as secondary narcolepsy, which can occur due to certain medical conditions or medications. Here's an overview of each type:
1. Narcolepsy Type 1 (with Cataplexy):
o This is the classic form of narcolepsy.
o It is characterized by the presence of cataplexy, which is a sudden and temporary loss of muscle tone triggered by strong emotions like laughter, anger, or excitement.
o Individuals with narcolepsy type 1 often experience excessive daytime sleepiness, sleep attacks (sudden and uncontrollable episodes of falling asleep), and disrupted nighttime sleep.
o Other common symptoms may include sleep paralysis (inability to move or speak while falling asleep or waking up), hypnagogic hallucinations (vivid and dream-like hallucinations when falling asleep), and disrupted nighttime sleep.
2. Narcolepsy Type 2 (without Cataplexy):
o This type of narcolepsy lacks cataplexy, which is the hallmark symptom of narcolepsy type 1.
o People with narcolepsy type 2 still experience excessive daytime sleepiness and may have sleep attacks, sleep paralysis, hypnagogic hallucinations, and disrupted nighttime sleep.
o However, the absence of cataplexy differentiates it from narcolepsy type 1.
3. Secondary Narcolepsy:
o Secondary narcolepsy is less common than narcolepsy type 1 and type 2.
o It can result from other medical conditions or factors, such as brain injuries, tumors, or certain medications.
o The symptoms of secondary narcolepsy can be similar to those of narcolepsy type 1 or type 2, but they are usually attributed to an underlying medical cause.
Symptoms of narcolepsy
Narcolepsy is a neurological disorder that affects a person's ability to regulate sleep-wake cycles. Its primary symptom is excessive daytime sleepiness (EDS), but it can also involve other symptoms and features. Here are some common symptoms and characteristics of narcolepsy:
1. Excessive Daytime Sleepiness (EDS): People with narcolepsy often experience overwhelming daytime sleepiness, which can lead to frequent and uncontrollable episodes of falling asleep during activities such as working, studying, or driving.
2. Cataplexy: Cataplexy is a sudden loss of muscle tone triggered by strong emotions, such as laughter, anger, surprise, or excitement. It can range from mild muscle weakness to complete muscle paralysis, causing individuals to collapse. Not everyone with narcolepsy experiences cataplexy.
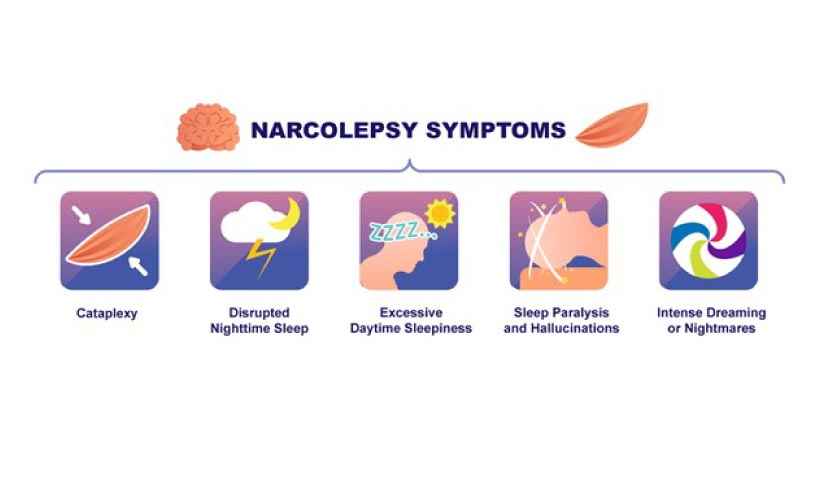
3. Sleep Paralysis: Sleep paralysis is the temporary inability to move or speak upon waking up or falling asleep. It can be a frightening experience and is often accompanied by vivid hallucinations.
4. Hypnagogic Hallucinations: These are vivid and often frightening hallucinations that occur when falling asleep or waking up. These hallucinations can involve visual, auditory, or sensory experiences.
5. Fragmented Sleep: People with narcolepsy may experience disrupted nighttime sleep, waking up frequently throughout the night or having difficulty staying asleep.
6. Automatic Behaviors: During episodes of excessive daytime sleepiness, individuals with narcolepsy may continue to perform routine tasks or activities, but they do so on "autopilot" without full awareness.
7. Irregular Sleep Patterns: Narcolepsy can disrupt normal sleep-wake patterns, leading to irregular sleep cycles and a tendency to take short naps throughout the day.
8. Insomnia: Some individuals with narcolepsy may experience difficulty falling asleep or staying asleep at night.
What causes narcolepsy?
The exact cause of narcolepsy is not fully understood, it is believed to involve a combination of genetic, environmental, and autoimmune factors. Here are some of the leading theories and factors associated with narcolepsy:
1. Genetic Factors: Narcolepsy tends to run in families, suggesting a genetic component. Certain genes have been linked to narcolepsy, particularly those related to the regulation of the neurotransmitter hypocretin (also known as orexin). Hypocretin is involved in promoting wakefulness, and a deficiency in this neurotransmitter is a key characteristic of narcolepsy.
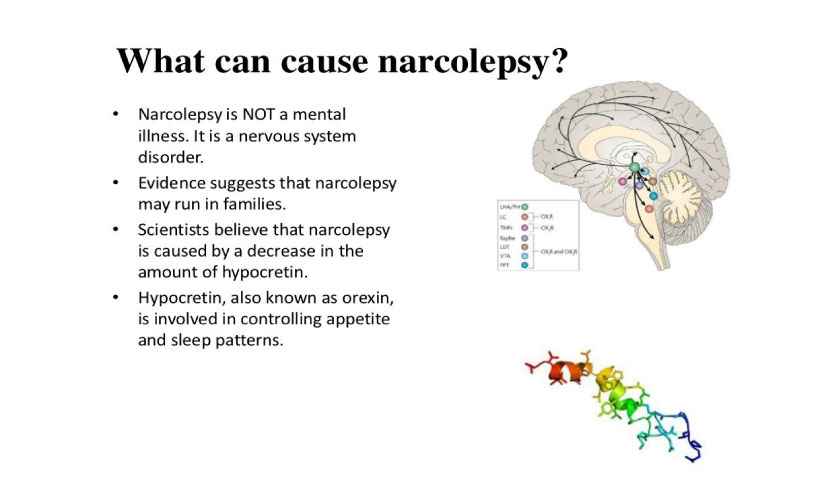
2. Autoimmune Response: One prominent theory is that narcolepsy may result from an autoimmune response. In some cases, the body's immune system may mistakenly attack and destroy the cells that produce hypocretin in the brain. This autoimmune response is thought to be triggered by environmental factors, such as infections (e.g., streptococcal infections) or other unknown triggers.
3. Brain Abnormalities: Some research suggests that there may be structural or functional abnormalities in certain regions of the brain that are involved in sleep-wake regulation. These abnormalities may contribute to the development of narcolepsy.
4. Neurochemical Imbalance: Narcolepsy is associated with disturbances in the balance of neurotransmitters in the brain. In addition to hypocretin, other neurotransmitters like serotonin and dopamine are also believed to play a role in narcolepsy.
It's important to note that narcolepsy is a complex disorder with varying degrees of severity and different symptoms. The exact cause and mechanisms may vary among individuals, and further research is ongoing to better understand this condition.
Is narcolepsy a disability?
Narcolepsy can be considered a disability, but whether it is officially classified as a disability and the extent to which it affects an individual's life and functioning can vary widely from person to person. Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness, sudden episodes of muscle weakness (cataplexy), sleep paralysis, and vivid hallucinations when falling asleep or waking up.
In many countries, including the United States, narcolepsy may qualify as a disability under certain conditions. For example, the Americans with Disabilities Act (ADA) in the U.S. prohibits discrimination against individuals with disabilities, and narcolepsy may be considered a disability if it substantially limits one or more major life activities, such as working, studying, or taking care of oneself.
To determine whether narcolepsy qualifies as a disability in a specific context, it often depends on the severity of the condition, how it impacts an individual's daily life, and the specific laws and regulations in place in a given jurisdiction. Many individuals with narcolepsy are able to manage their condition effectively with medication and lifestyle adjustments and continue to lead productive lives, while others may experience more severe symptoms that significantly affect their ability to work or engage in other activities.
If you or someone you know has narcolepsy and believes it may qualify as a disability, it is advisable to consult with a healthcare professional and, if necessary, seek legal advice to better understand the rights and accommodations available in your specific situation.
How is narcolepsy diagnosed?
Narcolepsy can often go undiagnosed or be misdiagnosed because its symptoms can overlap with other conditions. Diagnosing narcolepsy typically involves a combination of medical history evaluation, clinical assessment, and specialized tests. Here are the steps involved in diagnosing narcolepsy:
1. Medical History and Symptom Evaluation: The first step in diagnosing narcolepsy is a detailed medical history and symptom evaluation. A healthcare provider will ask you about your sleep patterns, daytime sleepiness, cataplexy (sudden muscle weakness or loss of muscle tone), sleep disturbances, and any other related symptoms.
2. Sleep Diary: Keeping a sleep diary for a few weeks can be helpful. You may be asked to record your sleep patterns, including when you go to bed, when you wake up, and any daytime naps. This information can provide valuable insights into your sleep-wake cycle.
3. Epworth Sleepiness Scale: Your healthcare provider may ask you to complete the Epworth Sleepiness Scale, a questionnaire that assesses your level of daytime sleepiness by asking you to rate your likelihood of falling asleep in various situations.
4. Polysomnography (PSG): A polysomnogram is an overnight sleep study conducted in a sleep clinic. During PSG, several physiological parameters are monitored, including brain activity (EEG), eye movements (EOG), muscle activity (EMG), heart rate, and breathing. This test helps identify any sleep disorders, such as sleep apnea, that might be contributing to your symptoms.
5. Multiple Sleep Latency Test (MSLT): The MSLT is usually conducted the day after the PSG. It measures your daytime sleepiness by assessing how quickly you fall asleep during several short naps scheduled throughout the day. People with narcolepsy often have a shorter time to sleep onset during these naps, which is a key diagnostic criteria.
6. HLA Typing: A blood test to determine your human leukocyte antigen (HLA) type, specifically HLA-DQB1*06:02, can be used as a supporting diagnostic tool. Many people with narcolepsy have this genetic marker, though its absence does not rule out the condition.
7. Evaluation for Cataplexy: If you experience cataplexy (sudden muscle weakness or paralysis triggered by emotions), your healthcare provider will assess this symptom as part of the diagnosis. A clinical evaluation and detailed medical history can help confirm the presence of cataplexy.
8. Exclusion of Other Conditions: It's important to rule out other medical or psychiatric conditions that can mimic narcolepsy symptoms. Conditions such as sleep apnea, restless leg syndrome, and certain mood disorders can have overlapping symptoms.
Once all the necessary information and test results have been collected, your healthcare provider can make a diagnosis based on the criteria outlined in the International Classification of Sleep Disorders (ICSD-3). If narcolepsy is confirmed, a treatment plan can be developed to manage the condition, which may include lifestyle changes, medication, and behavioral therapy.
Do I have narcolepsy?
I'm not a medical professional, and I can't diagnose medical conditions. If you suspect you may have narcolepsy or are experiencing symptoms of narcolepsy, I strongly recommend that you consult a healthcare provider. They can evaluate your symptoms, medical history, and potentially perform tests to make an accurate diagnosis. Common symptoms of narcolepsy include excessive daytime sleepiness, sudden and uncontrollable episodes of falling asleep (called "sleep attacks"), cataplexy (sudden loss of muscle tone), and vivid hallucinations upon falling asleep or waking up. Only a healthcare professional can provide you with a proper diagnosis and treatment plan if necessary. Please seek medical advice for your specific situation.
Treatment for narcolepsy
The treatment for narcolepsy typically involves a combination of medications and lifestyle adjustments to help manage the symptoms. Here are some common approaches to treating narcolepsy:
1. Medications:
o Stimulants: These are often the first line of treatment and help to reduce excessive daytime sleepiness. Examples include modafinil (Provigil) and armodafinil (Nuvigil). Methylphenidate and amphetamine-based medications may also be prescribed in some cases.
o Sodium Oxybate (Xyrem): This medication is effective in reducing both daytime sleepiness and cataplexy. It's usually taken at night in two doses and can improve nighttime sleep quality.
o Selective Serotonin and Norepinephrine Reuptake Inhibitors (SSNRIs): Medications like venlafaxine or duloxetine may be used to treat cataplexy.
o Tricyclic Antidepressants: Medications like imipramine or clomipramine can also help manage cataplexy and improve nighttime sleep.
2. Lifestyle Adjustments:
o Scheduled Naps: Short, planned naps during the day can help manage excessive sleepiness.
o Regular Sleep Schedule: Maintaining a consistent sleep schedule, even on weekends, can help regulate your sleep-wake cycle.
o Avoiding Triggers: Identifying and avoiding factors that worsen symptoms, such as alcohol and caffeine close to bedtime, can be helpful.
o Exercise: Regular physical activity can improve sleep quality and overall well-being.
o Healthy Diet: A balanced diet can help regulate energy levels and promote better sleep.
3. Behavioral Therapies:
o Cognitive Behavioral Therapy (CBT): CBT can help address the psychological aspects of narcolepsy, such as anxiety and depression, which often accompany the condition.
4. Supportive Therapies:
o Support groups or counseling can provide emotional support and help individuals cope with the challenges of narcolepsy.
5. Safety Precautions:
o Because narcolepsy can lead to sudden and unexpected episodes of sleepiness, individuals with narcolepsy should take precautions when driving or operating heavy machinery.
It's important to note that the treatment approach may vary from person to person, and it may take some time to find the right combination of medications and lifestyle adjustments that work best for an individual. Additionally, individuals with narcolepsy should work closely with a healthcare provider experienced in treating sleep disorders to develop a personalized treatment plan. Regular follow-up appointments are essential to monitor progress and make necessary adjustments to the treatment regimen.
Medication for narcolepsy
Narcolepsy is typically a lifelong condition, and while there is no cure, medication and lifestyle adjustments can help manage the symptoms. Treatment for narcolepsy often involves a combination of medication and behavioral therapies. Here are some medications commonly used to treat narcolepsy:
1. Stimulants: Stimulant medications are the primary treatment for excessive daytime sleepiness in narcolepsy. They help increase wakefulness and alertness. Commonly prescribed stimulants include:
o Modafinil (Provigil)
o Armodafinil (Nuvigil)
o Methylphenidate (Ritalin)
o Amphetamine-based medications like dextroamphetamine (Adderall)
2. Sodium Oxybate (Xyrem): This medication is often used to treat cataplexy and excessive daytime sleepiness in narcolepsy. It is taken at night and helps improve sleep quality, reduce nighttime awakenings, and decrease daytime sleepiness.
3. Selective Serotonin Reuptake Inhibitors (SSRIs): Certain SSRIs, such as fluoxetine (Prozac), sertraline (Zoloft), and venlafaxine (Effexor), can be used to manage cataplexy and improve REM sleep symptoms.
4. Tricyclic Antidepressants (TCAs): TCAs like imipramine (Tofranil) and clomipramine (Anafranil) can also be used to treat cataplexy.
5. Wake-Promoting Agents: Other wake-promoting agents like solriamfetol (Sunosi) may be prescribed to help manage excessive daytime sleepiness.
6. Antidepressants: In some cases, certain antidepressants, such as venlafaxine or atomoxetine, may be used to manage narcoleptic symptoms.
It's essential to work closely with a healthcare provider or sleep specialist to determine the most suitable medication for your specific narcolepsy symptoms. Medication management may require regular adjustments to find the right balance between symptom control and managing potential side effects.